It’s not breaking news that communicating with the public is vital for the success of your schools. And you know all too well that your relationship with local media can affect the way your community perceives you—and how often your story gets told.
We get it. Sometimes it’s hard to trust that the media has the purest intentions. News is a business, after all, and the most positive things happening on your campuses won’t always strike a reporter as newsworthy material.
As you know, no matter the story, your obligation is to the public. The media’s biggest concern is holding you to that. This can often make it seem like the press is an opposing force to your schools, only wanting to sell stories or get a good scoop. But this is a huge misconception, and it could be keeping you from sharing the most impactful stories coming out of your district.
“Don’t overthink it,” advises Alia Malik, an education reporter for the San Antonio Express-News. “Don’t think of it as one journalist or one media outlet. When you talk to the media, you’re talking to the public. Treat us with the same respect you would treat them.”
We know you can’t control every piece of news that’s out there about your schools—and that can be scary. What you can control is how you approach and work with the media. By building strong, trusting relationships with local education reporters, you can keep the most accurate stories about your schools in the news cycle and ensure you’re being heard in times of celebration or distress.
Beginning a media strategy can seem daunting. However, education reporters are actually looking for stories to print on schools, and they need credible sources to make their stories stronger. So what can you do to make sure they’re contacting your district?
Jenny LaCoste-Caputo knows a thing or two about building partnerships with the media. Before becoming the Chief of Public Affairs and Communications for Round Rock ISD in Texas, she was an education reporter herself. LaCoste-Caputo’s experience in journalism has helped her build a thriving partnership between her district and local media in the Austin area.
“When I was a reporter, I would often get frustrated with communications folks. I would say, They just don’t understand what we need,” she tells SchoolCEO. “You have to understand, frankly, that journalists are not your PR agency; that’s not their job. Their job is to report the news, to be a watchdog for the public.”
No matter how tempting it may seem, funneling inspiring stories to the media probably won’t get your schools the coverage you’re seeking. They may appreciate a celebratory story here and there, but touting your district’s strengths just isn’t their job—and this false expectation could lead to frustration for everyone.
Instead, make it your goal to build goodwill with local education reporters. When they’re on a deadline, you want them calling your district to ask for quotes and clarification—not asking a neighboring district or publishing a story without your knowledge. If the media knows you’re a good source to work with, you can start reaping the rewards of those partnerships. Once you’ve had a few conversations with your local media outlet, you’ll start to pick up on their needs—which puts you in a perfect position to supply information.
Make the initial connection.
To foster a good relationship with local media, connect with them before there’s a big story—when you don’t need anything at all. Get to know who’s reporting on your schools: not just who they are, but how they work, how they communicate, and what they expect from you and your team.
(Click here to read the full story.)
Making that initial connection with a reporter doesn’t have to be scary, either. Remember that it not only benefits your schools, but also helps journalists who may be looking for education stories to cover down the line. The reporters we talked to said they appreciated school communications personnel reaching out to them directly—through email, phone call, or even text message.
“You’re almost always better off if you make a personal connection with someone,” says Charles Lussier. He’s been reporting on education for The Advocate in Baton Rouge, Louisiana, for 19 years. “If the goal is to actually get coverage, there needs to be a meeting of the minds. It’s harder and harder because there are fewer and fewer folks like me, and there are more and more schools seeking attention.”
He recommends reaching out to reporters with a simple email introduction. “Sometimes that could just be, Hey, do you have a minute to chat about what may work for you and what won’t?” he advises. “I get a lot of cold call emails where there is no connection made at all. Anybody who covers your schools on a daily or weekly basis is someone you’ll want to get to know.”
According to LaCoste-Caputo, establishing these personal connections should be a priority. “The very first thing you do is start to establish those relationships, calling reporters, telling them a little about yourself,” she says. “Try to set up coffee or lunch with them. Meetings are great—phone calls are fine too. But if you can start building a relationship, that’s always going to be helpful. Someone’s far more likely to pick up the phone or respond to your email if they recognize your name when they see it come across the screen.”
Let them know your “why.”
Even though the media is never going to be your PR agency, articulating your vision for the district can help them tell the complete story of your schools. If a journalist understands your mission, they’ll better understand your choices; they’ll get to know you. Eventually, they might even pick up on some of the words you are using in your marketing and branding—and help tell your district’s story.
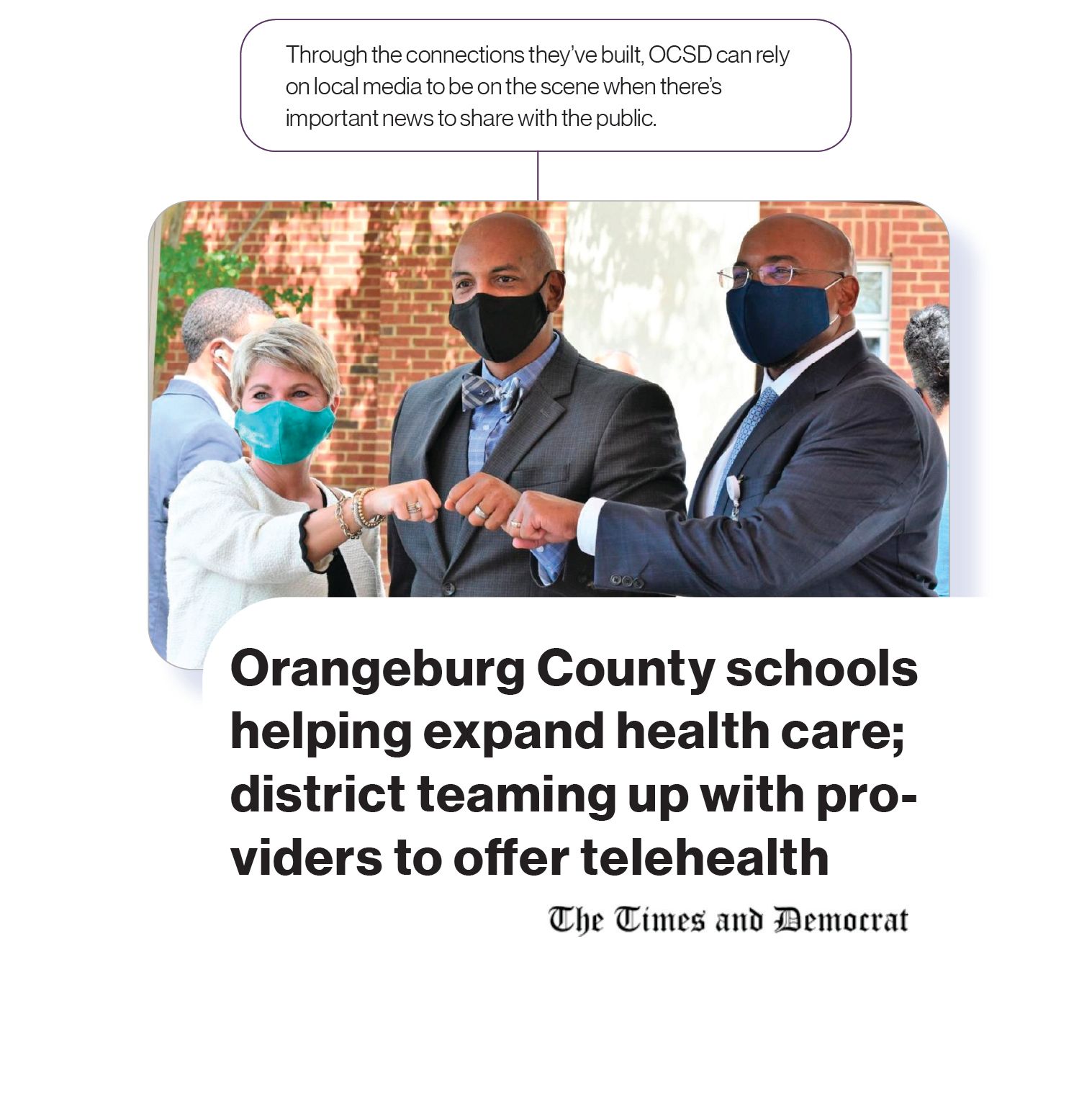
For Dr. Shawn Foster, new superintendent of Orangeburg County School District in South Carolina, making a thoughtful connection with local media has allowed him to share his mindset as a school and community leader. “I think it’s important, first of all, that you sit down and explain your philosophy,” he tells us. “As superintendents, we have to make sure people see the big picture in regards to communication, because education is no longer about just reading, writing, and arithmetic. Education is a foundational economic driver for communities. We determine if someone’s going to come live here, if businesses are going to come in—we determine all of those things. So the message about your schools that the media puts out impacts everyone that lives in that community, including that media entity.”
Dr. Foster also stresses that a strong relationship with the media is beneficial in making sure who they’re writing about and reporting on is never forgotten. “We have to tell a story about children,” he says. “That’s the one thing people have to remember when you’re talking about communication in the school aspect—you’re talking about kids. No matter where they go when they leave us, if someone hears something negative about the area they come from, people oftentimes unfairly associate what they heard with those kids. And that’s not fair to them. So it’s extremely important, because a child may have to bear the burden of what we put out into this small world.”
Building and Maintaining Credibility
Let’s say you’ve put in the work: you’ve reached out to local media, had coffee chats and Zoom calls, exchanged emails and phone numbers. You trust that when a story comes their way, you’ll be the first to know. But how do you maintain that level of credibility when things get chaotic or unpredictable? How can you ensure that you’re still trusted to be a reliable source, no matter the news?
Maintaining your credibility is an essential part of your relationship with the media and the public. “If you’re working with the same school comms directors for any length of time, you have a sense of who’s responsive and who’s capable of getting your questions answered,” Malik tells us. “If you don’t return calls and you’re not interested, that doesn’t let you off the hook. When the school district is not releasing or providing that information, then that becomes part of the story.”
Credibility can also go a long way with the media in times of crisis. We know it can be difficult to be responsive when your priority is the safety and health of your students and staff, so that foundation of trust can go a long way with a journalist. If you know a reporter and they know you, the communication between you will be more timely, efficient, and accurate. The relationship you’ve already built with them saves you drama and stress when your schools need you most.
There are three main tenets to maintaining credibility: be responsive, be prepared, and be transparent.
Be responsive.
Remember that reporters are busy, and they’re often working on a deadline. You don’t have to respond perfectly, but make sure that you respond as soon as possible.
(Click here to read the full story.)
“Reporters are really busy just like we’re all really busy,” LaCoste-Caputo tells us. “So being specific and brief is really important. If you take the time to build those relationships, here’s what’s awesome—on slow news days when they’re looking for something, they’re going to call you up, because they trust your judgment and know you’ll hustle to churn something out quickly.”
Be prepared.
One thing you don’t want slowing you down when dealing with the press is not knowing about state or local laws, especially concerning media relations with the district. “I think comms directors need to have some basic knowledge about public records and open meetings laws in their states,” says Malik. “They shouldn’t have to go to their district’s lawyers every single time there’s a media request.”
This is another reason it’s especially important for a school leader and their communications director to work closely together. “I think the comms person and the super need to have a symbiotic relationship themselves,” Lussier tells us. “The comms directors who are more plugged in are the ones I seek out. Reporters always prefer to talk to people who are in the know.”
(Click here to read the full story.)
Be transparent.
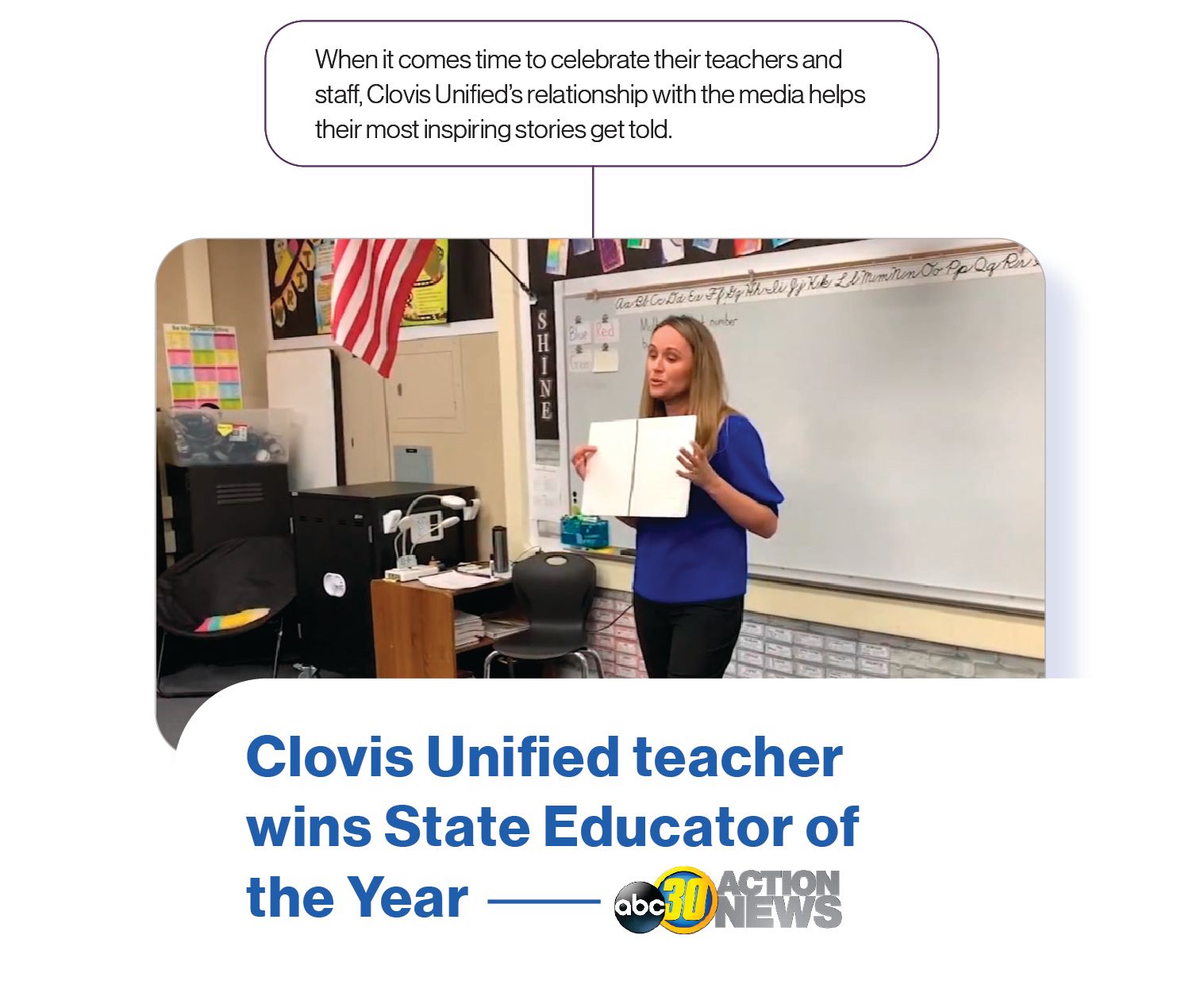
Transparency is the foundation of your credibility, and the experts we spoke with emphasized it repeatedly. “If the media feels like you’re going to hide things from them or answer in a misleading way, they will not trust what you’re sharing with them,” says Kelly Avants, APR, former President of NSPRA and current Chief Communications Officer for California’s Clovis Unified School District. “It’s a huge one—be transparent and be willing to rip off your own Band-Aid.”
In San Antonio, Malik covers education in an area with 17 public school districts and more than 30 private and charter schools. Needless to say, she knows a few things about keeping up healthy relationships with school districts. “Good comms directors tell the truth and are open and transparent,” she says. “I understand they have lots of demands on their time, but I think they should prioritize talking to the media because they view it as talking with the public.”
Being honest and forthright regarding your district is not just a way to build credibility and strengthen your brand—it’s your obligation to the public. “You want to make sure to have an organization that’s doing things the right way,” LaCoste-Caputo says. “But then also share the challenges. People need to understand them. It’s two-fold. You’re building trust for being honest. But primarily, you’re demonstrating your needs so that when there’s a call to action, people feel compelled to answer.”
Pitching Stories
We don’t have to tell you that newsworthy things are happening on your campuses every single day. But without a strategic and thoughtful plan for collecting and sharing these stories, you could be missing out on countless chances to connect with your community and highlight your schools through media coverage.
The media won’t always know what’s going on in your schools unless you tell them. So you also need a plan for taking stories you’ve collected from your schools and pitching them to local education reporters. With an internal story pitching strategy and a plan for pitching to the media, you can be sure the best things happening in your schools don’t go unnoticed.
Create an internal system for pitching stories.
Nobody knows your schools better than the teachers and administrators in your classrooms everyday. But if a class starts a successful fundraiser for a local food bank, would their teacher know how to share that story with the district or media? Does the principal know who to talk to? Should they go to your communications team or directly to the media?
“Our district has some pretty strict protocols in place, and I think for a leader who is learning or rethinking their media strategy, there’s a lot of value in that,” says Avants. At Clovis Unified, she assigns a communications liaison to each one of the district’s more than 50 school sites. This person serves as the district’s eyes and ears on the ground. “They’re tasked with sending information to us,” she explains. “They’re bringing that content to us, and we’re figuring out how to use it—maybe putting out a press release, creating a media event, or simply posting a video on Instagram. We consider ourselves our own newsroom in a sense. We certainly work with the media to tell our story, but it is incumbent on us to tell our own story as well.”
Many journalists don’t like the idea of checking in through the communications office before talking with sources in schools, but Avants says there are good reasons to do this as a district. “I often remind the media that we are sometimes dealing with contentious custodial issues with families who have restraining orders, one parent against the other, etc.,” she says. “We want to be confident that our systems are not going to put a vulnerable child in the line of a camera or a reporter that would be jeopardizing them while they are under our care.”
So as you align your district’s media communications, make sure your stakeholders know that there are always extenuating circumstances and events that are beyond anyone’s control. Make sure they know your system is meant to help them communicate their stories, not silence them. “There’s some time lost in unnecessary middleman stuff if there’s restrictions on teachers reaching out to the press,” says Malik. “What I’m concerned about is that people feel like they are able to talk to the press no matter where they fall in the school system—especially students and their families.”
In Orangeburg County, students and families always come first when it comes to communication with the media. For Merry Glenne Piccolino—Orangeburg’s Assistant Superintendent for Communications, Business, and Community Partnerships—that means having a solid system in place that helps find the most impactful stories to share. “Alignment is important to me,” she tells us. “I think about a teacher being an example of a strategic vision for the school district. When you can actually have a human interest story that relates and contributes to the vision and the goals of the school district and shows its employees fulfilling that vision, it’s such a win.”
So you’ve got your plan in place for gathering story pitches from your schools, but how do you take those ideas and share them with the media? Unfortunately, you can’t just send them anything that comes across your desk—you need to learn more about their needs and what they like to cover. What are they looking for in terms of stories?
(Click here to read the full story.)
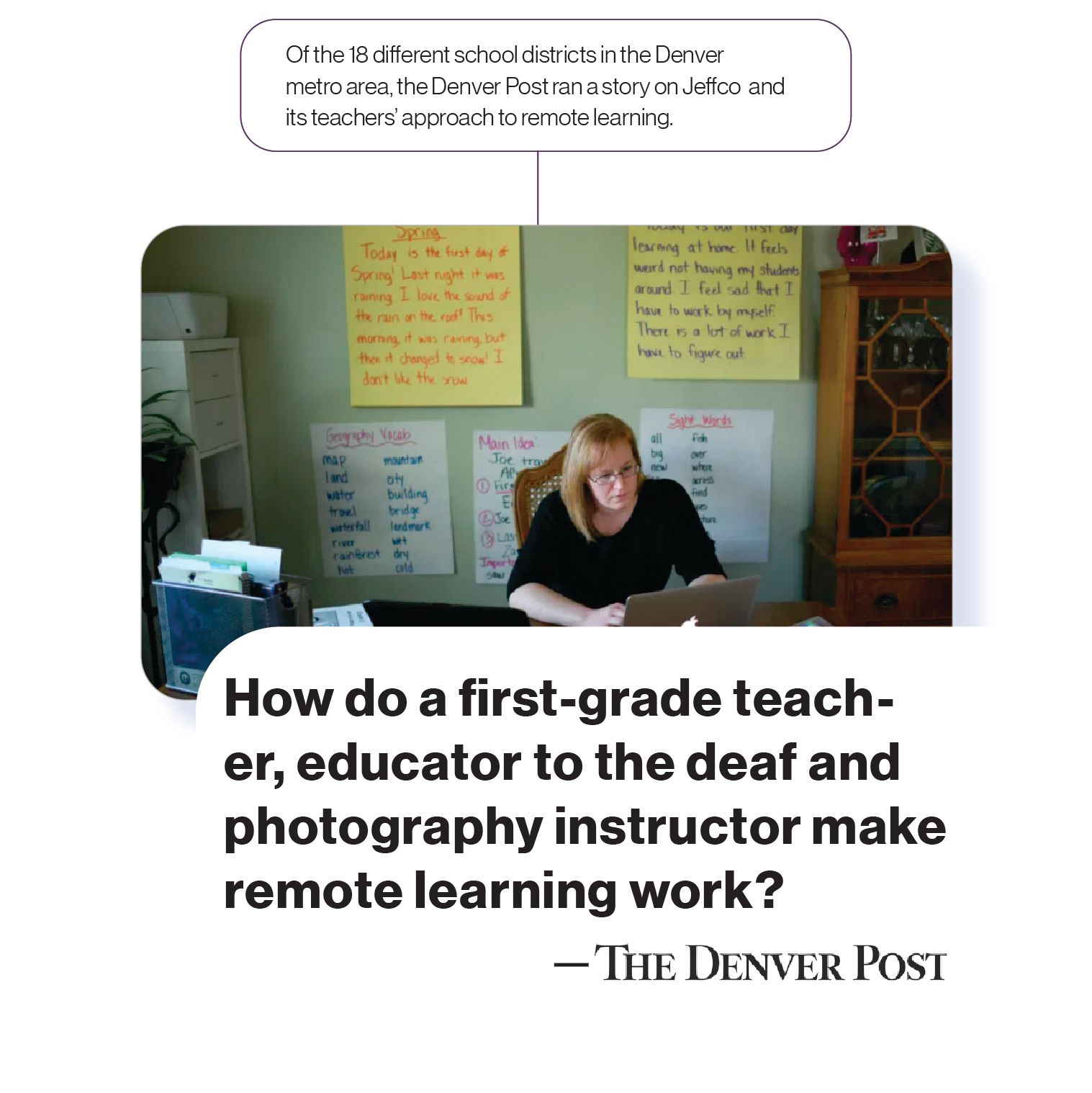
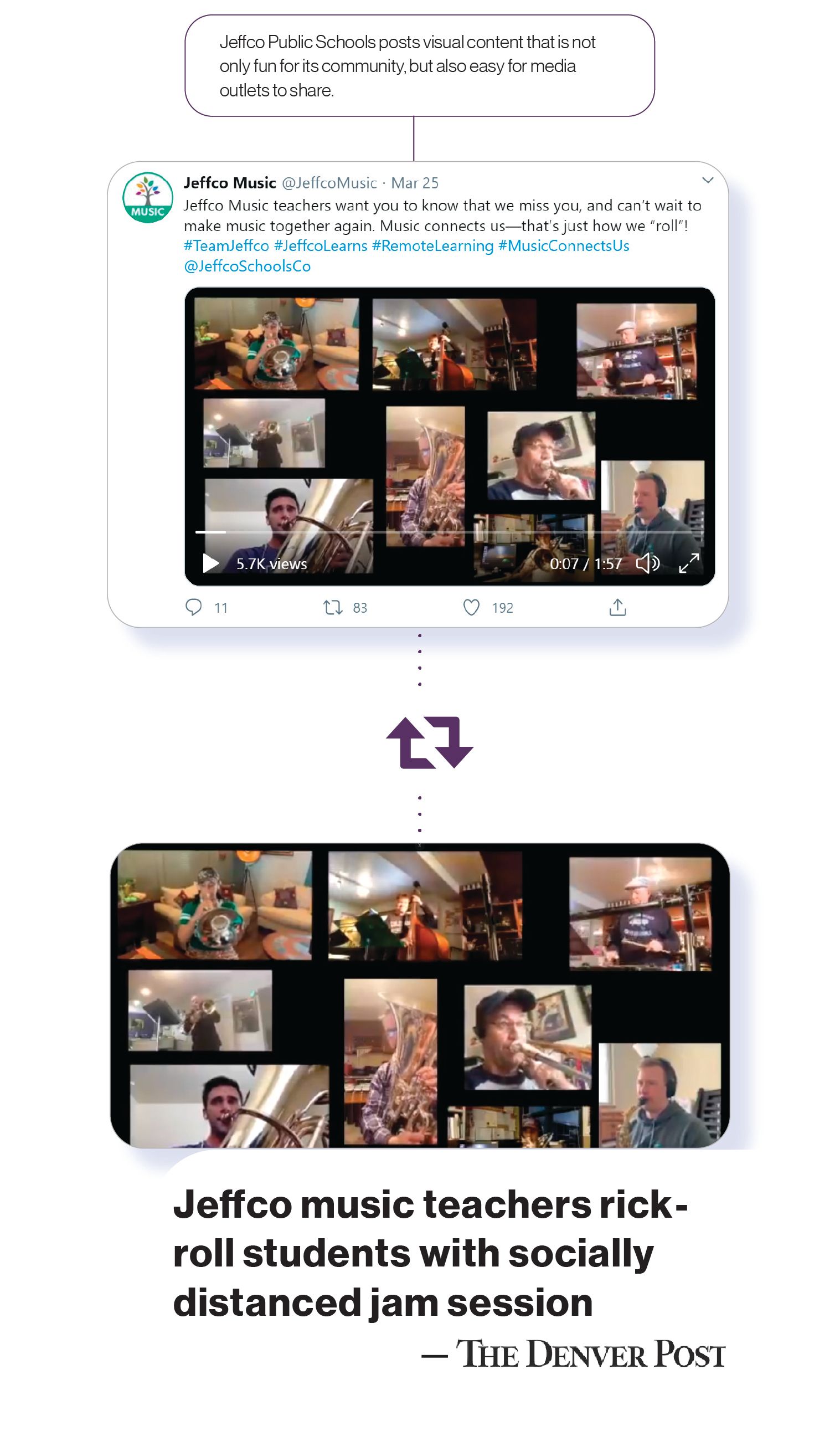
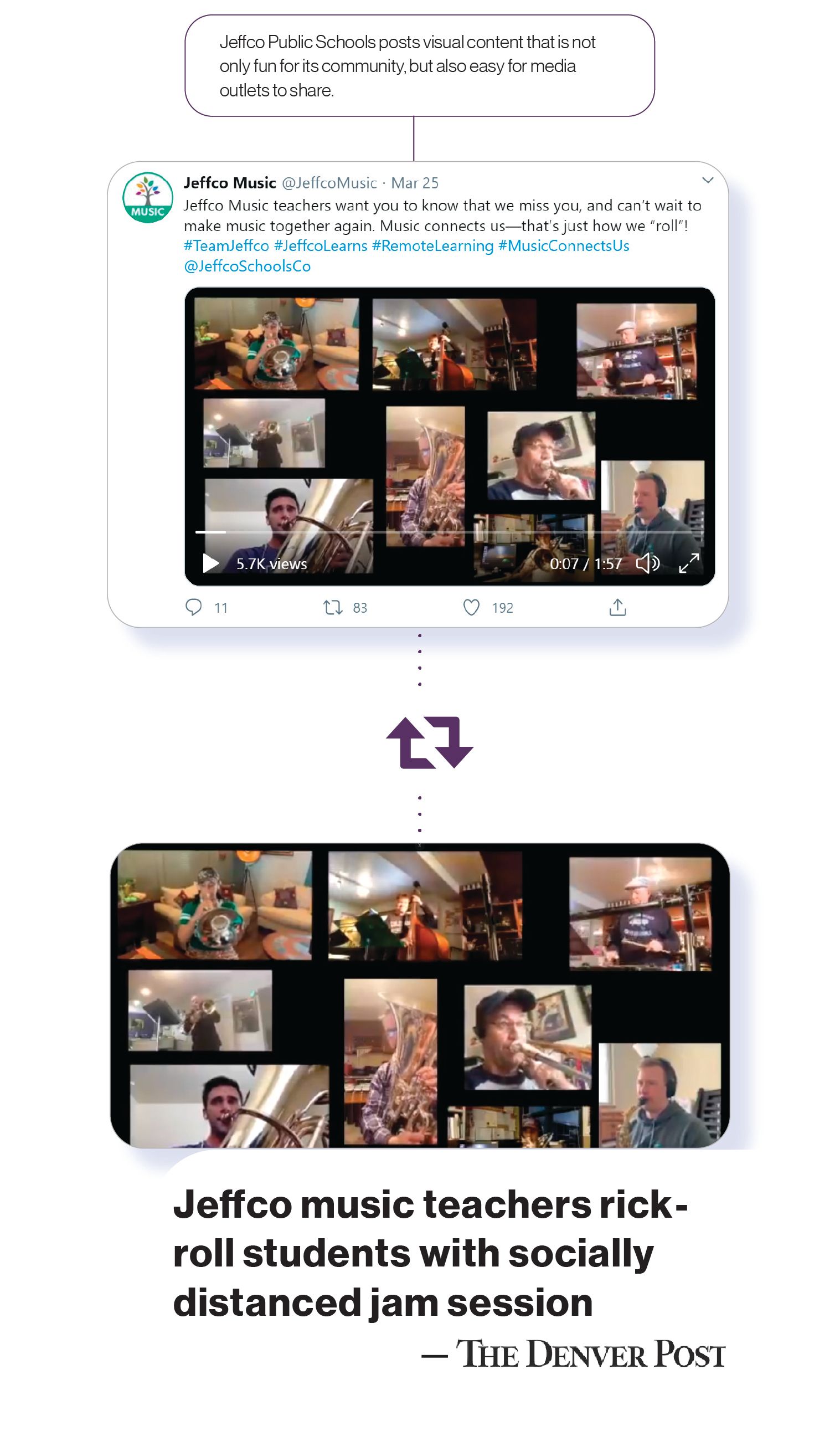
Cameron Bell, Executive Director of Media Relations and Public Information for Jeffco Public Schools in Colorado, does research into her district’s local media to learn as much as she can about them. “Get to know publications and outlets,” she advises. “Watch them, read them, follow them on social media—and follow reporters on their own channels as well. Look at what they’re doing so you can also get to know them. That way, you know their voices and what they tend to report on most often. You know what kind of stories they like to tell and seem passionate about.”
Bell also says to be aware that some journalists you work with may not know exactly what they’re looking for. “A lot of reporters who normally cover politics or sports are having to cover things like education because of shortages,” Bell tells us. “A lot of them will say to me, I don’t even know what this means. Can you help me?” If you’re prepared with newsworthy stories and pitches, you can make a reporter’s job a lot easier—and that buys you goodwill and helps you build a stronger connection.
However, the media is always looking for a few common things. “People need to think in terms of what is new, what is a little different,” says Lussier. “They also need to think about the medium. I work at a newspaper. Newspapers aren’t just print entities anymore; we’re news sites. So we’re also trying videos now. The more complete the package on a story you can deliver to someone like me, the more it’s sellable. Especially if it’s visual.”
Education is rife with confusing and complicated rhetoric, so it’s also important to keep that in mind when you’re pitching a story. “The more complex a story, the more human you’ve got to make it,” Lussier advises. “If readers see someone grappling with something in real time and in real circumstances, it’s going to mean more, and it’s going to come alive.”
Knowing what your local media is looking for in terms of education stories will make things a lot less stressful for you, your communications team, and the media. And if everyone’s on the same page, the right stories get told.
Don’t be afraid to nudge reporters.
Depending on your location, you may or may not be dealing with a great number of other schools that want to tell their stories, too. Keeping up your end of the communication bargain may sometimes mean being consistent and assertive in pitching to the media to make sure you’re being heard.
In Jeffco, Bell sends out a weekly newsletter to local media that includes a list of story pitches from schools around the district. “Once I send them out, I post each one on our media relations webpage,” she says. “We give information, but we also pitch fun stories, give construction updates, and things like that.” When directly pitching to a reporter, Bell may use “a blurb-like pitch” or even develop an idea into a story that a reporter can then expand on.
It also never hurts to follow up with a reporter or reach out when something is important or timely. “Definitely nudge me,” Lussier says. “If you really think something is a story, you may have to grab me by the lapel and shake me a little bit and go, This is something and here’s why. Don’t assume that I’m just going to jump to it. If I’ve been doing five other things, it wasn’t even on my radar.”
In terms of how you should nudge or reach out to a reporter, Lussier offers some sound advice. “It’s usually an escalation. If it’s something happening now, give me a call. If it’s something happening tomorrow or the next day, you can start with an email or maybe send a text.” Also remember that reaching out to a reporter who may be too busy for your story isn’t a fruitless endeavor. “If I can’t do it, but I know it’s something big enough, I may be able to find someone else, or we can think about a plan B and circle back,” he says.
When Bad News Strikes
Your schools should be prepared to respond to any kind of story that comes across a reporter’s desk. Sometimes, as you well know, it isn’t good news. So first it’s important to acknowledge and accept that you can’t keep news from reaching your community, no matter what it’s about. Because you serve the public, much like the media, you already know that being transparent and responsive is a top priority. This, in turn, will help you build strong relationships with local education reporters so that when negative things do happen, they call you first.
React thoughtfully and honestly.
As simple as it may seem, being thoughtful goes a long way, and being as honest as possible with the media and public should always be your priority. If there’s a story involving your schools, you want local media to know they can trust you to give them the answers. Bad things happen every day, and you certainly don’t want your reaction to the media to become part of the story.
“Realize that anytime someone has an issue, they’re going to call me,” Lussier tells us. “But if I have a good relationship with a district, I’m not going to pop off with the first tip of the day. I’m going to call them and go, Look, I heard about this. What’s going on here? I’m willing to have a conversation with them on anything people come to me with.”
To react to negative stories in a thoughtful, transparent way, be as open as you can be with the media and public about whatever is going on. If there’s been an incident on one of your campuses, or a mistake has been made, your district should be as upfront as possible. “There are going to be negative things that happen,” Piccolino says. “The media needs to know that when we’ve done something wrong, I’m going to own it. I’m not going to sugarcoat it or try to spin the story or anything like that. If a child is hurt or something else has happened that is the fault of an employee, process, or system, I’m going to own it, apologize, and identify how we’re going to do things differently to prevent it from ever happening again.”
Build a bank of good stories.
You can’t keep bad things from happening, but you should always remember that good things are happening, too. Having a system in your schools for gathering those inspiring stories means you’ll be ready to share them when you need to most.
“We’re always trying to build that bank of really good stories,” Piccolino says. “We’re one of the largest employers in the community, and people make mistakes—kids, adults, everybody. Sometimes when things aren’t going so well, we pull a story out of our pocket that is going to change hearts and minds. Those living examples help refocus the community’s mindset on what’s positive and on the intentions of our work. It recenters public interest and attention on something that is positive so that stakeholders can put a small error in perspective while remembering the larger and overwhelmingly positive impact our school system makes.”

(Click here to read the full story.)
By being prepared to share your very best stories, you can ensure that no matter what happens, your schools are being seen, heard, and understood. As the saying goes, If you don’t tell your story, someone else will. After all, it’s the media’s job. But nobody ever said you couldn’t help them along the way.

SchoolCEO is free for K-12 school leaders. Subscribe below to have a digital copy of the most recent edition of SchoolCEO sent to your inbox.


 “People connect no matter what, right? The more you start talking to someone and the more you know them and the more you engage, the screen just kind of falls away.”
“People connect no matter what, right? The more you start talking to someone and the more you know them and the more you engage, the screen just kind of falls away.”



 Loraine Daugherty is Chief Executive Officer at
Loraine Daugherty is Chief Executive Officer at 