CARES Act provider relief payments disproportionately went to medically underserved areas, helping providers in already struggling areas to keep their doors open during the peak of lockdowns.
– At the start of the COVID-19 pandemic, the healthcare industry was confused, scrambling, and scared. Patients did not know when and where it was safe to seek care and providers were overwhelmed with patients needing care for a disease they did not know how to treat. Hospitals quickly hit capacity as ICU beds filled with patients needing ventilators while small physician practices had to close because no patients were coming in for care.
The Coronavirus Aid, Relief, and Economic Security (CARES) Act provided economic stimulus and relief throughout the country amidst the COVID-19 pandemic and gave specific funding directly to providers and care delivery organizations. In total, this Provider Relief Fund allocated over $50 billion to Medicare fee-for-service providers for healthcare-related expenses or lost revenue as a result of COVID-19.
As telehealth quickly emerged as a catch-all solution to providers many challenges, Provider Relief Funding could support providers implementing these solutions without seeing a drop in revenue. Supportive policies from CMS and other payers relaxed restrictions previously limiting telehealth’s use and funded telehealth-based care.
Primary care visits delivered via telehealth grew by nearly fifty percent. But providers still needed support to rollout telehealth solutions and other technologies that improved patient access to care and kept safety at the forefront of care delivery. Providers needed to innovate if they were to keep their doors open and adjust practice to meet the demands of the time.
Funding from the CARES Act gave providers a needed economic boost when patient volume was at an all-time low and provide support to rolling out solutions that would keep facilities operating. An additional $18 billion was set aside for Medicaid and CHIP providers, including assisted living facilities. A final $20 billion was allocated for financial losses and changes in operating expenses to providers including, behavioral health providers.

A portion of the Provider Relief Fund was distributed based on the provider’s 2018 Medicare fee-for-service revenue. Additional funding was granted based on provider application, so those providers who were leveraging value-based payments were also eligible for funding.
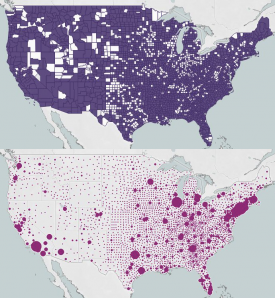
New York, California, and Texas received the highest total number of payments across all states, according to the Department of Health and Human Services (HHS). Allocation strategy indicated that the areas hit the hardest by the COVID-19 pandemic would receive priority payment.
Over 40,000 payments were given to California providers alone, as this state has the highest number total cases across the county at over 1.5 million, according to data from the Centers for Disease Control and Prevention.
Payments ranged from $1 to $1,196,544,217 but averaged $265,759 for all recipients. HHS appeared to live up to its call as those areas hit the hardest by the COVID-19 pandemic received some of the highest payments.
But medically underserved areas also appear to have received higher total payments and average payments from the Provider Relief Fund than their counterparts in resource-rich areas, revealed an analysis from Xtelligent Healthcare Media.
Medically underserved areas are defined by the Health Resource and Services Administration (HRSA) as geographic areas that lack access to primary care services. Four elements contribute to an area being designated as a medically underserved area:
- Rate of primary care providers
- Percent of population at the federal poverty level
- Percent of population over age 65
- Infant mortality rate
A low rate of primary care providers for an area means patients have difficulty accessing care where and when they need it.
As primary care is central to care delivery and often the spoke behind care coordination, limited access to these services and results in poor care delivery and uncoordinated care. Previous research has shown that populations with a high proportion of primary care providers see lower mortality rates and improved life expectancy.
Poverty rates have also long been tied to health outcomes. Social determinants of health such as income and economic opportunity can correspond to a slew of health-related factors from accessibility of care to access to safe housing, all of which impact health outcomes.
Population over the age of 65 is likely also considered an element in the medically underserved designation as older patient populations typically have higher rates of comorbidities and chronic conditions.
These conditions, including diabetes and heart disease, require more and more frequent health services. A higher population over the age of 65 would suggest a stressed healthcare system or at least a healthcare system needing more resources to care for a sicker population.
Similarly, high infant mortality rate suggests poorer health status of mothers and thinned healthcare resources.
So medically underserved areas have the perfect storm of overextended care – fewer providers to care for a greater and more in-need patient population. These areas are in greater need of assistance to meet these needs of their complex patient population.
It is, therefore, reassuring that analysis from Xtelligent Healthcare Media found 240,461 more Provider Relief Fund payments made to providers in medically underserved communities.
Data on provider payments from HHS was paired with the HRSA’s indication of medically underserved populations to understand the relationship between relief payments and county-level resources.
The average payment for providers in medically underserved areas was over $20,000 higher than those in resource-rich environments. Not only does this data indicate that those areas in the greatest need received more payments, but they also received higher valued payments.
The difference in total payments to medically underserved areas compared to non-medically underserved areas was over $66 billion.
While reassuring that providers the most in need of additional resources were receiving aid, this data does not reflect the total impact of Provider Relief Funding in these communities because the data is only based on the payments accepted by providers at the time of analysis. Pending payments were not a part of analysis and reports from July show that nearly $100 billion had yet to be dispensed. Hopefully, this pending aid will continue supporting providers who are already stretched thin because of resource limitations in their communities and the impact of COVID-19 on their practice.
While priority was given to areas hit the hardest by COVID-19, the current wave of infections is sweeping the country irrespective of state and county lines. How HHS dispenses the remaining funds will be critical to support providers in areas with the most need.
It is a positive indication that medically underserved counties received over $66 billion more in aid than non-medically underserved populations, but is this enough?
For providers in areas where broadband is limited, HHS funding may not be enough to support equal access to telehealth services for their entire patient population. Or cancer care clinics whose patients are at the highest risk for developing severe COVID-19 may not have enough funding to provide safe and effective home care. Continued support to these areas will be critical moving forward as the pandemic continues to sweep the country.

