Dr. Raed Azzam, an epileptologist with the Cleveland Clinic Neurological Institute, talks with a patient during a telemedicine appointment at his office at the Cleveland Clinic Akron General Wellness Center in March. While telehealth appointments aren’t new, they’re being used with greater frequency because of the COVID-19 pandemic, especially for mental health services, and are likely here to stay.
After a year of talking with patients via Zoom, phone and sometimes FaceTime, some mental health providers are confident that telemedicine is here to stay, even after the pandemic goes away.
Kristen Carpenter, director of ambulatory services at Ohio State Harding Hospital, said the hospital did some telehealth services before the pandemic, but it mostly was used to connect different emergency rooms and to provide emergency psychiatric care. But with COVID-19, the hospital went from providing “almost 100 percent in-person care to almost 100 percent care via telehealth” almost immediately, she said.
Now, with about 90 percent of Harding’s outpatient care still provided via telehealth, Carpenter said she foresees a future where patients can choose how they’d like to receive their care.
“Our patients have experienced almost no interruption in their care,” she said. “We have been able to provide care that we never thought we could do via telehealth.”
Harding currently offers individual counseling and psychiatry services in person and via telehealth. Its partial hospitalization and intensive outpatient program — a structured three- to four-week treatment program that typically requires patients to attend full-day group sessions in the hospital — now takes place over Zoom.
John Dawson, interim president and CEO of Community for New Direction in Columbus, Ohio, also sees telemedicine in the nonprofit group’s future — even though it had offered no telehealth services before the pandemic.
“We have a higher show rate. There’s so many barriers to mental health and substance use disorder patients getting to appointments that telehealth has helped tremendously in that area,” he said.
A new study finds during the first few months of the pandemic, patients were more likely to use telehealth services for behavioral health treatment than physical conditions, according to a January study published recently by RAND Corp. The study shows that 53.6 percent of patients with a behavioral health condition sought treatment via telehealth from mid-March to early May of 2020. By comparison, 43.2 percent of patients with a chronic physical condition used telehealth to receive care during the same period.
Providing services via phone or video conferencing has broken down many barriers including unreliable access to transportation and work conflicts, Carpenter said. At Harding, for example, there are fewer emergency cancellations and lower no-show rates because of telehealth appointments, she said.
As with other things provided remotely, however, there are some drawbacks.
Linda Jakes, executive director of Concord Counseling Services in Westerville, Ohio, said the nonprofit group found it a bit more difficult in particular o treat young children and older adults remotely. Both groups tend to be more difficult to engage, she said, and older adults sometimes have more trouble navigating technology than other patients.
“It could be difficult when you’re just having a phone conversation with someone to really see the body language associated,” Jakes said. “There’s a lot of things that we use our eyes for.”
There are other challenges as well, said Dawson of Community for New Direction.
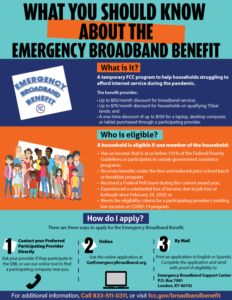
Having reliable internet and access to a private space for appointments are privileges that some people simply don’t have, he said.
To address telehealth accessibility, he said his agency is working to provide funding for data cards and phones for patients in need.
Aside from accessibility, some patients must be seen in person, Dawson said. Those include individuals with severe opiate use disorder or personality disorders, for instance, who require closer assessment. All patients, he added, come into the office for their intake paperwork and subsequent drug tests, if it is part of their treatment plan.
Concord Counseling has established safety protocols such as staggered appointment times and alternating days that employees come in, but otherwise is letting individual clinicians decide when they want to bring patients into the office, said Mike Preston, director of clinical operation. He said most providers have in-person appointments with patients for whom “telehealth is just not working for them.”
Carpenter said having mostly virtual appointments has been draining for providers, who sit in front of computer screens for hours at a time without breaks. And though mental health treatment lends itself to telehealth, the social interaction that in-person care provides is lost in virtual appointments.
“As the year has progressed, we’ve focused a lot on how coming into the office can actually be a kind of intervention for behavioral health, to draw them back out into the world,” she said.
Jakes said telehealth has been invaluable and she can’t imagine returning to offering only in-person care. But she said many clinicians are looking forward to certain milestones that they didn’t appreciate before the pandemic.
“I was talking to one of our therapists the other day and she goes, ‘Oh my God, it’s going to be so exciting to come back,’ because she has a chunk of her caseload that she’s never even met, she’s only done telehealth,” Jakes said. “She goes, ‘If I passed them on the street, I wouldn’t even know who they are.’”